2021 – 2026 | HRSA Funded Program
Program Objectives
The Harvard Medical School Center for Primary Care developed the ECHO+ model to equip primary care practitioners in rural areas with the resources needed to provide high-quality specialty care, and sustain these efforts through incorporation of a QI framework.
The ECHO+ model incorporates evidence-based telementoring and case conference elements of Project ECHO, with robust didactic learning through formal HMS certificate courses developed and taught by HMS faculty. QI is taught in parallel using the innovative Sprint model (a focused model for rapid-cycle change) and sites choose metrics based on the clinical topics to improve and follow.
A Pathway for Expansion
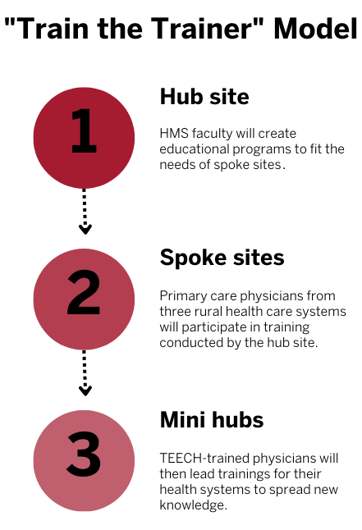
Using a “Train-the-Trainer” method, the Center serves as the “hub site” and rural health sites initially serve as “spoke sites” that are located in health professional shortage areas. Rural PCPs practicing at the spoke sites are trained in the first sixteen months of the program on clinic topics identified based on need, alongside the QI process. Then they function as “mini-hubs” to disseminate their knowledge and QI approaches to other rural primary care providers (doctors, nurses, etc.), both at their clinic and elsewhere, creating a pathway for expansion.
Partnering Spoke Sites
There are three partnering spoke sites participating in TEECH.
- ARcare – A large federally qualified health center with clinic sites in Arkansas, Kentucky and Mississippi
- Chickasaw Nation – A federally-recognized tribe with a medical center and tribal clinics in Oklahoma
- Minnie Hamilton Health System – Which contains a FQHC and a Rural Health Clinic in West Virginia.



Health Care Needs of the Target Population
The partner spoke sites provide care to rural populations that are disproportionately impacted by chronic diseases. The clinic sites are predominately fully or partially located in primary care, dental and behavioral health care health professional shortage areas (HPSAs). These rural populations face the following conditions:
-
High levels of poverty and unemployment
-
Low levels of educational attainment and literacy
-
Increased social determinants of health needs
-
Access barriers (geographic isolation, lack of public transit)
-
Higher levels of chronic diseases including cardiovascular and pulmonary diseases