As COVID-19 continues to wreak havoc—infecting more than 33 million people globally—it has also caused significant disruptions in eye health services, with a particular emphasis on ophthalmologic care for cataracts. This disruption is alarming, especially since untreated cataracts are the leading cause of blindness globally, affecting nearly 20 million people.
Notably, healthcare delivery has dramatically changed throughout the course of the COVID pandemic; many clinics have closed, staying open for emergency services only. And these changes have affected ophthalmology services, resulting in delayed eye appointments, postponed surgeries, and restriction of clinical consults to patients with emergent eye conditions. Further, the shift towards telehealth eye care is a feasible alternative for some people, though the International Agency for the Prevention of Blindness states that telehealth can disenfranchise those who live in remote locations without access to technology.
If these eye care delivery trends continue, eye health could be compromised globally, leading to millions with visual disabilities.
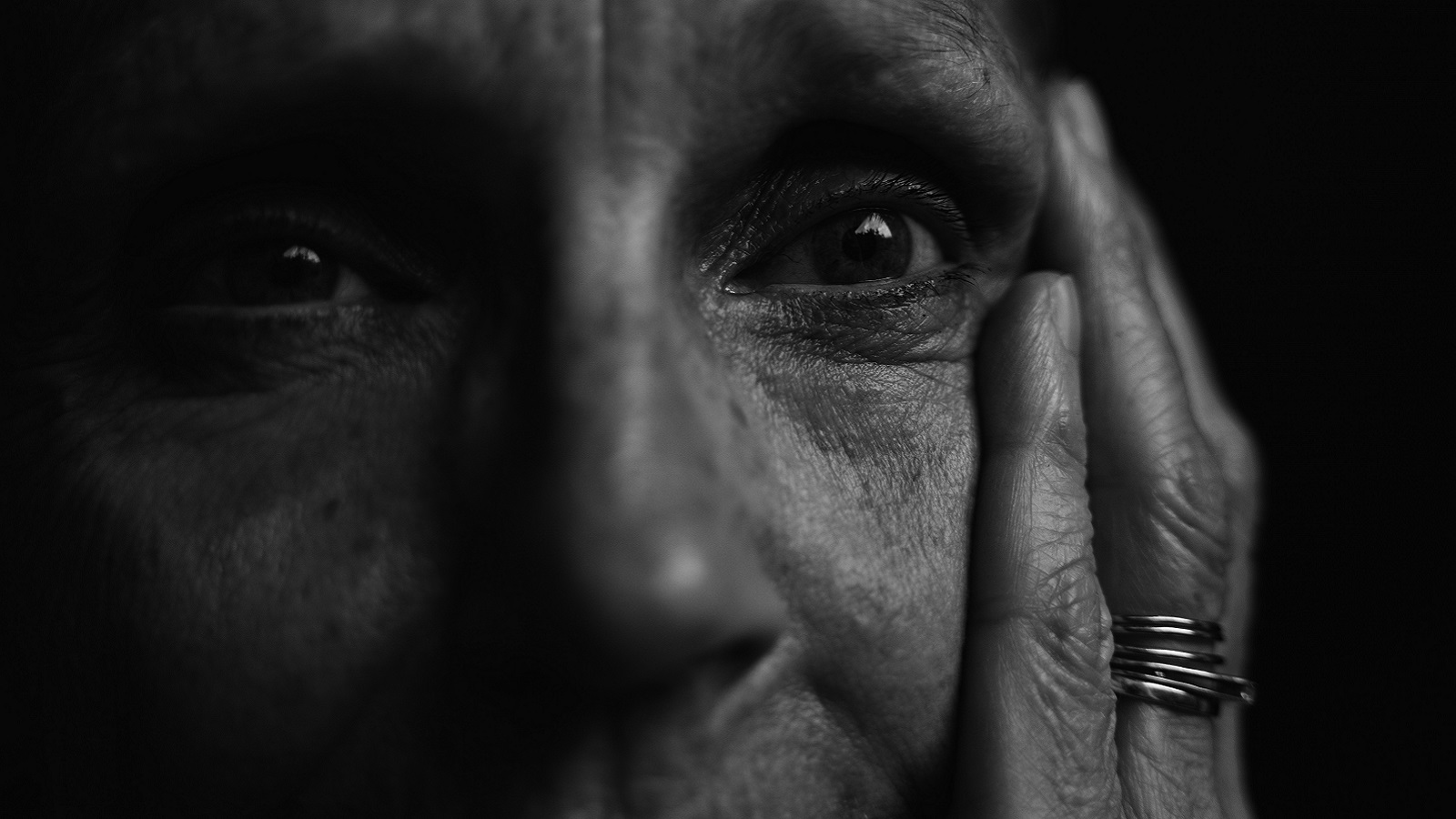
Cataracts are a global challenge, leading to blindness for millions… and this loss of sight seriously impacts our ability to live life to the fullest. And further, elderly people are often most affected by cataracts. Because older age is also associated with higher risk for severe COVID infection, this results in anxiety regarding cataract surgery during the COVID pandemic—a difficult decision between regaining sight and evading infection with the potentially deadly coronavirus.
In the United Kingdom, recent research shows that 65% of patients on a cataract surgery waitlist report their poor eyesight significantly interferes with quality of life, yet 37% of them are willing to wait until the end of the COVID pandemic to undergo cataract surgery in order to avoid coronavirus exposure and transmission. Moreover, poor vision can restrict movement within homes, resulting in isolation, limited independence, anxiety, and depression.
COVID is here to stay for many more months, and patients with cataracts cannot afford to wait indefinitely. To promote equity, services must go on while ensuring the utmost safety for both patients and health professionals. We recommend three ways to help achieve this:
- Eye doctors should stay connected with their patients remotely to ensure they have the proper medications and adequate supply, understand how to use each medication, and check-in regarding any complications or concerns. We recommend home visits for all patients who cannot be reached remotely, and we emphasize the importance of strict COVID protective measures during these visits. Telehealth eye care and home visits (when necessary) allow eye doctors to identify emergency cases and to also provide palliative eye care pending surgical removal of cataracts.
- Because cataracts negatively affect quality of life and can result in mental health consequences, it’s also necessary to address mental health during remote eye care visits. Because of the stigma associated with mental health—like the EpiAFRIC and Africa Polling Institute research that showed Nigerians believe mental health disease is caused by possession of evil spirits (54%) and punishment by God (23%)—it is critical that ophthalmic mental health counselors inquire about patients’ emotional well-being. And further, patients’ families and caregivers should be educated about mental health, especially regarding when and how to request professional mental health support.
- For patients who require emergency services, eye doctors should have detailed, effective, and streamlined COVID-related protocols in order to ensure the safety of all patients and health workers. Based on an analysis by Amnesty International, COVID-19 has resulted in the death of more than 7,000 health workers globally, thus demonstrating the urgent need for proper safety protocols for all in-person healthcare delivery.
As our world comes together to fight the pandemic, it is critical that we practice these eye care measures now in order to ameliorate a blindness pandemic that lasts far beyond the COVID-19 crisis.
**Feature photo by Matej from Pexels
Interested in other articles like this? Subscribe to our newsletter

Ifeanyi M. Nsofor, MBBS, MCommH, is a Medical Doctor and Masters in Community Health graduate from the Liverpool School of Tropical Medicine. Ifeanyi is a Senior Atlantic Fellow for Health Equity at George Washington University, Senior New Voices Fellow at the Aspen Institute, and CEO of EpiAFRIC.
 Shubha Nagesh, MBBS, MHA, is a Medical Doctor, Director of Community Follow-up & Research at The Latika Roy Foundation in Dehradun, India, and global health advocate for disabled children. She is a Senior Atlantic Fellow for Health Equity at George Washington University.
Shubha Nagesh, MBBS, MHA, is a Medical Doctor, Director of Community Follow-up & Research at The Latika Roy Foundation in Dehradun, India, and global health advocate for disabled children. She is a Senior Atlantic Fellow for Health Equity at George Washington University.
- Share
-
Permalink