Access to comprehensive primary care has long been a challenge in the United States, and the economic and social impacts of the COVID-19 pandemic will have far reaching implications on our healthcare system. Sixty percent of Americans have at least one chronic condition, and many patients have complex needs that require additional coordination, time and resources than what traditional models of care provide.
Physical distancing policies and the conversion to virtual health, while important for reducing COVID-19 transmission, threatens maintenance of routine care when virtual health does not adapt to meet the capacity and needs of diverse patient populations. Disruptions in care for patients with complex medical and psychiatric co-morbidities can result in adverse events, particularly when coupled with the emotional stress brought on by a public health crisis. COVID-19 requires that providers completely rethink their care models to keep patients healthy at home.
The federal government is currently making significant investments in telehealth and has softened regulations and payment policies to remove barriers during this emergency period. While this crisis presents an opportunity to galvanize operational improvements in how we deliver primary care to all patients, we must be careful to not inadvertently create obstacles for patients to access the care they need. We need to better understand both patient and clinic readiness to engage in this type of care in order to invest appropriately to support effective implementation.
Leveraging the crisis response to create lasting change
If implemented strategically, population health concepts, behavioral health integration and telehealth deployed during the COVID-19 response can serve to increase access for vulnerable populations far beyond the pandemic. The COVID-19 response has created the conditions necessary to accelerate the move to effective telehealth in primary care. Patients and providers are much more willing to try, and barriers to virtual care have been removed, at least temporarily (e.g. softer HIPAA rules, relaxed reimbursement parameters).
The ability to manage patient populations remotely requires a comprehensive transformation:
- virtual communication with the entire health team
- creative staffing models
- outreach and protection for vulnerable populations
- telehealth visits
- behavioral health integration
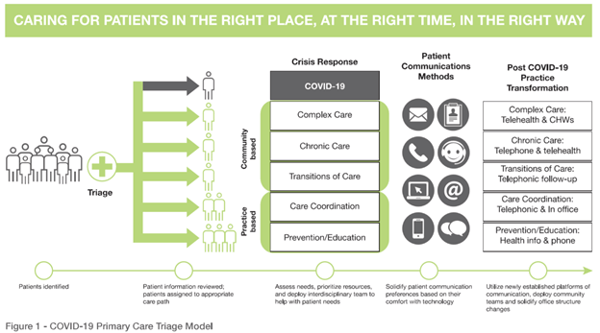
The pandemic response requires that healthcare systems now triage and manage medical needs through remote systems and specialized facilities. If disease prevention, education and behavioral health services were not being handled through virtual communication before, they are now. Such systemic changes accelerate the move to safer, more convenient access to care, and can become the basis for permanent alterations to operations and communication.
Rethinking patient-provider communication models
Crisis communications in health systems are generally coordinated and pushed out from marketing and public relations departments to reach the masses through mediums like the media, email, websites and social media sites. We can leverage communication streams being built and used for patient populations now to tailor future messages, education and virtual care to what works best for individual patients.
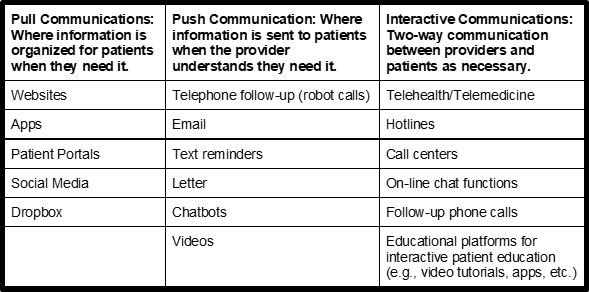
In the midst of the pandemic, primary care providers are deploying telehealth, behavioral health interventions, crisis lines, nurse help lines, patient portal communication, interactive chatbots, email, text communications and a variety of online teaching tools to remotely meet patient needs. Many of these changes can be utilized for lasting primary care transformation, such as the following tools:
Primary care has a tall order to maintain and promote population health, which has become even more apparent during the COVID-19 pandemic. The following table outlines how virtual communication and telehealth can be utilized to maximize access to primary care:
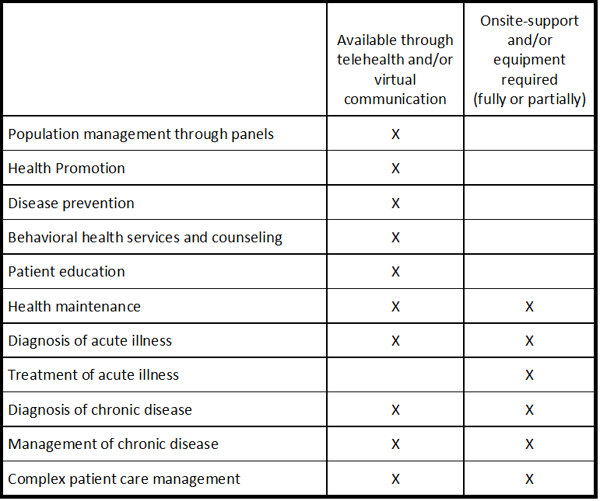
Primary care providers have acted quickly to enable these capabilities. However, significant investments need to be made to understand patient access needs, enable virtual communication and telehealth capacity for organizations, re-establish workflows and workforce capacity to function with these new methods and keep patients engaged in their health.
Importantly, each patient’s healthcare needs are different, and not all care can be provided remotely. For patients with limited capacity for virtual communication, as well as those whom require in-person visits during the pandemic, creating thorough triage systems, workflow “swimlanes” and distancing of care is a critical component to safe practice. In order to do this, patients need to be assessed from both the clinical as well as social determinants of health perspectives, including the capacity for virtual communication. Based on this information, patients can be triaged to different workflows. For example, complex care patients who aren’t yet ready to engage via telehealth may benefit from home visits by community health workers. The following virtual health readiness assessment tool is designed to identify and triage patients based on their healthcare and psychosocial needs:
The COVID-19 pandemic has provided the elements to accelerate a complete transformation in our primary care system, though additional investments are necessary to adequately address the needs of our most vulnerable patients. We must hardwire the transformation taking place during this public health crisis to build a more resilient primary care infrastructure that meets the preventive and chronic care needs of diverse patient populations. Appropriate investments that enable support for the adoption of patient-centric policies are essential to enabling safe and healthy communities now and in the future.
Acknowledgements: Thank you to Rosemarie Day for contributing thought partnership on this piece.
**Feature photo obtained with standard license on Shutterstock.
Interested in contributing to the Harvard Primary Care Blog? Review our submission guidelines
Interested in other articles like this? Subscribe to our bi-weekly newsletter
 María Fernanda Levis, MPH, MPA, is CEO of Impactivo, a social impact consulting firm with the mission of transforming health systems. She has been Principal Investigator and/or Project Lead under awards from the National Science Foundation, Health Resources and Services Administration, CDC Foundation, and the Patient-Centered Outcomes Research Institute. She holds a Master of Public Administration (MPA) & Master of Public Health (MPH) from Harvard University, Certification as Data Science Manager from John Hopkins University, and recognition as Patient-Centered Medical Home (PCMH) Content Expert from the National Coalition for Quality Assurance.
María Fernanda Levis, MPH, MPA, is CEO of Impactivo, a social impact consulting firm with the mission of transforming health systems. She has been Principal Investigator and/or Project Lead under awards from the National Science Foundation, Health Resources and Services Administration, CDC Foundation, and the Patient-Centered Outcomes Research Institute. She holds a Master of Public Administration (MPA) & Master of Public Health (MPH) from Harvard University, Certification as Data Science Manager from John Hopkins University, and recognition as Patient-Centered Medical Home (PCMH) Content Expert from the National Coalition for Quality Assurance.
 Lara Shadwick, MBA, is an Affiliate Consultant at Day Health Strategies. Prior to that, Lara was the Program Director at Mountain-Pacific Quality Health, a CMS-contracted Quality Improvement Network, where she developed a complex care program to address high needs, high-cost patients in rural settings.
Lara Shadwick, MBA, is an Affiliate Consultant at Day Health Strategies. Prior to that, Lara was the Program Director at Mountain-Pacific Quality Health, a CMS-contracted Quality Improvement Network, where she developed a complex care program to address high needs, high-cost patients in rural settings.
 Julie H. Levison, MD, MPH, MPhil, is an Assistant Professor at Harvard Medical School and board-certified in Internal Medicine and Infectious Disease. She is an NIH-funded Principal Investigator and has spent her career studying the impact of disease on society’s most vulnerable. Dr. Levison was a recipient of the El Planeta “Powermeter Award” (Top 100 most influential people for Latinos in Massachusetts) and the Arnold P. Gold Foundation Humanism in Medicine Award.
Julie H. Levison, MD, MPH, MPhil, is an Assistant Professor at Harvard Medical School and board-certified in Internal Medicine and Infectious Disease. She is an NIH-funded Principal Investigator and has spent her career studying the impact of disease on society’s most vulnerable. Dr. Levison was a recipient of the El Planeta “Powermeter Award” (Top 100 most influential people for Latinos in Massachusetts) and the Arnold P. Gold Foundation Humanism in Medicine Award.
 Sarah Bliss Matousek, PhD, MPH, contributes to strategic planning & implementation, change management, health reform, quantitative and qualitative research, operations, and program development. Dr. Matousek studied Health Policy & Management at Boston University School of Public Health and collaborated with a team at Harvard Medical School to develop and implement a mobile phone program for surgical patients in rural Haiti.
Sarah Bliss Matousek, PhD, MPH, contributes to strategic planning & implementation, change management, health reform, quantitative and qualitative research, operations, and program development. Dr. Matousek studied Health Policy & Management at Boston University School of Public Health and collaborated with a team at Harvard Medical School to develop and implement a mobile phone program for surgical patients in rural Haiti.
- Share
-
Permalink