Due to early misconceptions that COVID-19 didn’t lead to severe disease or death in children, US state surveillance dashboards were not set up to track the course of the pandemic among age-specific groups. Over time, state reporting for children has gradually improved, and The COVKID Project has been synthesizing and sharing data for children and teens since late April 2020.
Although 49 of 50 states now report COVID-19 case counts by age (with New York being the exception), only 2 states—Illinois and California—report cases for children and teens by race/ethnicity.
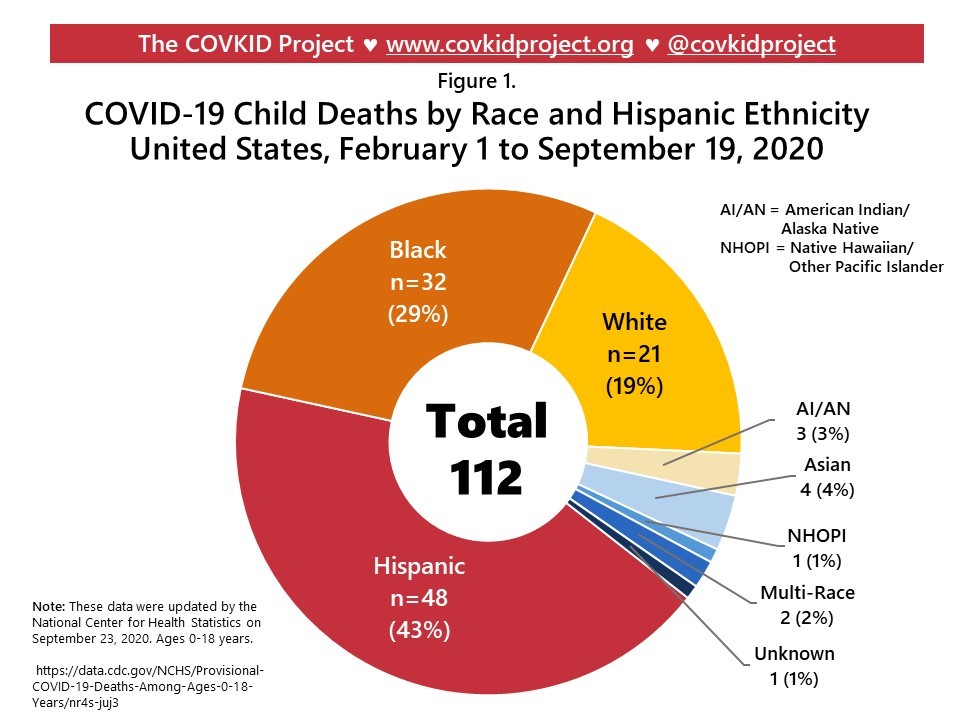
In August 2020, the National Center for Health Statistics began reporting nationwide provisional COVID-19 death counts by race/ethnicity for youth aged 0-18 years, as noted in Figure 1 below:
The COVKID Project has used these data to report population mortality rates for kids (through September 19, 2020), as noted in Figure 2 below:
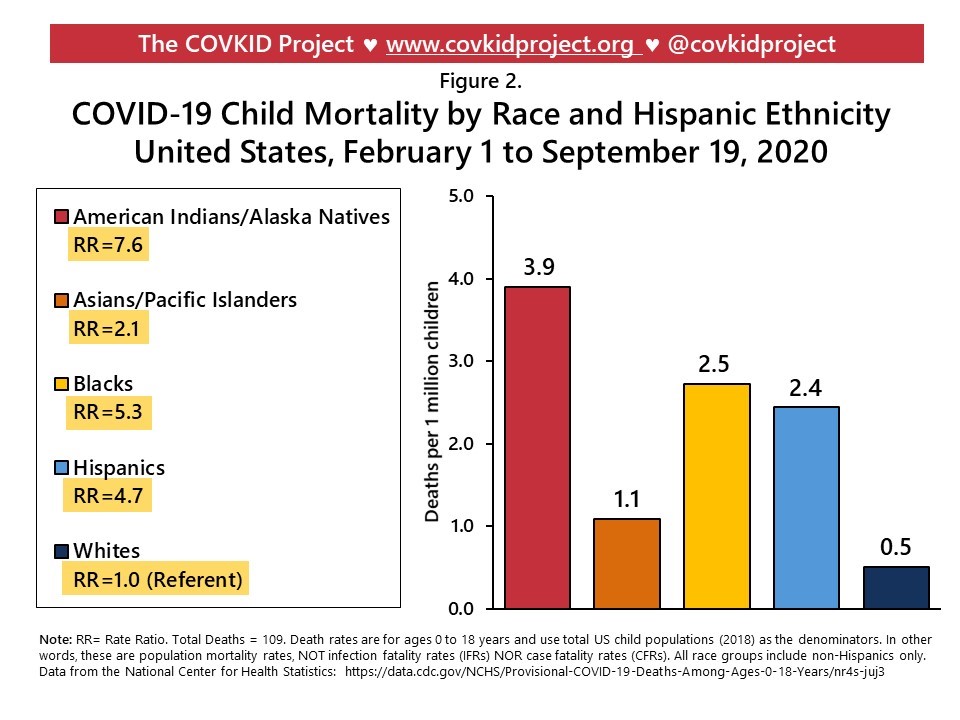
These mortality rates are relatively low, ranging from 0.5 to 3.9 deaths per million children, but racial/ethnic disparities are high. Compared to non-Hispanic white children:
- American Indian/Alaska Native (AI/AN) children are 7.6 times more likely to die from COVID-19;
- Black children are 5.3 times more likely to die;
- Hispanic children are 4.7 times more likely to die; and
- Asian and Pacific Islander children are 2.1 times more likely to die.
These and other disparities data are updated regularly on The COVKID Project Disparities Dashboard.
A new report from the Centers for Disease Control and Prevention (CDC) on 122 child deaths found that although AI/AN, Black, and Hispanic children represent 41% of the US population aged 0-20 years old, they accounted for 78% of COVID-related deaths in this study. Deaths were also more prevalent among males, youth aged 10-20 years, and 75% of decedents had at least one underlying condition.
Another finding from the CDC study was that 35% of youth deaths occurred in a hospital emergency department or outside of medical care completely. Deaths occurring in the absence of hospitalization represent a glaring deficit in access to healthcare, and particularly the life-saving aggressive interventions afforded by pediatric intensive care units (ICUs).
The primary drivers of racial/ethnic disparities in COVID-19 incidence include social, environmental, labor market, housing, and other socioeconomic factors. However, clinical trajectories of COVID-19 case severity and fatality are influenced by access to and quality of outpatient and inpatient care, infection severity, patient nutritional and medical vulnerabilities, and use of aggressive life-saving interventions for critically ill patients.
Reducing racial/ethnic disparities in COVID-19 mortality in children
COVID-19 infection is often completely asymptomatic in children. For some children, though, presenting symptoms may include sore throat, headache, nausea, diarrhea, or a wide variety of other somatic symptoms.
Emerging evidence suggests that certain nutritional and medical conditions can increase risk for a more severe disease course among children who are infected. Iron-deficiency anemia, diabetes, and obesity may increase risk for hospitalization, ICU admission, and death—and these conditions are more prevalent among low-income children and particularly, low-income Hispanic and Black children. Further, food insecurity contributes to both caloric overnutrition (overweight and obesity) and to nutrient-poor diets that result in deficiency conditions.
Food insecurity stems from the complex intersection of lack of affordable housing, low wages, high medical costs, social isolation, and other social determinants of health. Feeding America now estimates that 54 million Americans may experience food insecurity due to the effects of the COVID pandemic, including a potential 18 million children. And further, households with children are more likely to experience food insecurity.
Thus, clinicians should incorporate referrals to the Women, Infants, and Children Supplemental Food Program (WIC) into all pediatric encounters, regardless of perceived socioeconomic position of the family. In addition to supplemental food for infants and children aged 1-4 years, WIC also provides free nutrition assessments and education for parents and children.
For providers whose patient populations are predominately older adults, we recommend reassessment of employment status and occupation type, housing, and number of children and teens living in the home. Multi-generational households increase in parallel to economic hardship. Kids Count Data Center tracks the number of youth aged 0-18 years living in crowded households by city, state, and territory, providing helpful insights into community trends.
Addressing social determinants of health in the context of a clinic visit is a critical yet daunting task. The EveryOne Project offers a toolkit for the identification of health-related social needs, as well as resources for providers to advance health equity in their communities. A primary barrier to the improvement of care coordination is the lack of bidirectional information flow between healthcare settings and community resources. Integration of community resource referral information into the electronic medical record is key, but the adoption of technology varies widely. Aunt Bertha is one example of a social care network that tracks community resources in every US county and territory, and it’s also accessible via Epic.
COVID-19 prevention, screening, and severity mitigation for children will remain important for at least the next two to three years. And notably, there will not be a vaccine for the pediatric population for the foreseeable future, as no COVID-19 candidate vaccines are being tested in children. Thus, lasting amelioration of childhood mortality disparities in COVID-19 will require fundamental improvements in the socioeconomic and environmental determinants of health for Hispanic, Black, AI/AN, and Asian and Pacific Islander families.
About the authors

Elizabeth B. Pathak, PhD, MSPH, is an epidemiologist who has spent 30 years conducting research on geographic, socioeconomic, and racial disparities in health. She is a passionate advocate for methodologically rigorous scholarship which seeks to uncover the power relations that perpetuate socioeconomic and health inequities. She is Director of The COVKID Project and President of the Women’s Institute for Independent Social Enquiry.

Rebecca B. Garcia, MSN, FNP-C, CDE, is a family nurse practitioner and certified diabetes educator. She is Director of Regional Clinical Operations at Premise Health and a Healthcare Fellow with the Women’s Institute for Independent Social Enquiry. Her professional interests focus on social determinants of health, syndemics, COVID-19 return to work safety, decoding racial bias in practice, and lifestyle medicine.
**Feature photo by Aaron Burden on Unsplash
Interested in other articles like this? Subscribe to our newsletter.
Interested in contributing to Perspectives in Primary Care? Review our submission guidelines.- Share
-
Permalink

