As COVID-19 cases surge nationwide, routine and regular testing of asymptomatic people is being provided on an ad-hoc basis, without clear guidance from expert recommendations. In addition to personal protective equipment (PPE) and physical distancing, routine testing is being performed in many settings based on the observation that infected patients are contagious, despite not having symptoms, and could unknowingly pass the infection to others. Settings in which routine testing is commonly performed include college campuses and among residents of long-term care facilities. However, few healthcare settings are performing regular testing despite the fact that frontline healthcare personnel are at higher risk and could pass the infection to other healthcare workers and/or patients.
A recent article in Clinical Infectious Diseases, published by a research team that included the Harvard Medical School Center for Primary Care, analyzed (using simulation modeling methods) the research question of how often repeat asymptomatic surveillance testing (with PCR or high-sensitivity rapid antigen tests) would need to be performed among healthcare personnel to prevent transmission of the novel coronavirus in healthcare settings. Based on currently available national data, the research team simulated the following:
- Baseline incidence of infection of 0.5% per day;
- As many as 2.5 other people infected due to contact with each infected individual;
- 5-day incubation period during which an individual was infectious but asymptomatic (varied over time);
- Asymptomatic individuals being 50% as likely to transmit infection as those with symptoms; and
- A test that was 50-80% sensitive (also varying over the course of infection).
The research team found that to reduce the reproductive number (secondary cases caused by each infectious case) to fewer than one—which is needed to prevent or control an outbreak—routine testing would need to occur about twice weekly in most US clinical settings, with some variation depending on the sensitivity of the test and the rapidity of obtaining results. Testing asymptomatic people twice weekly would reduce the rate of others becoming infected by about 61%. In an analysis that tested the assumptions used in this analysis, the incidence of infection had little impact on the results. Both the sensitivity of the test and delays in reporting were important. The results were consistent with two other analyses—one in pre-print form and the other published in JAMA Network Open (focused on college campuses)—also indicating that testing every few days would be vital to preventing outbreaks.
Considerable logistical planning is needed to ensure that such frequent and reliable testing can be performed, but this challenge is surmountable. We specifically created a national testing network providing test results in less than 72 hours from rapid anterior nasal PCR tests (FDA-authorized, at-home kits). Significant detail was required for organizational leaders to participate in this network—far more detail than has been made available by the Centers for Disease Control and Prevention (CDC) or related state testing guidelines to operationalize rapid and frequent asymptomatic testing.
How would an organization know the right cadence of testing to minimize false positive results (common in low prevalence populations) while also minimizing the risk of a workplace outbreak? How much would the cadence need to change as community COVID-19 incidence changes and as a vaccine is rolled out, given that the vaccine will be imperfect and asymptomatic surveillance testing may still need to occur? Under what circumstances should rapid antigen tests with lower sensitivity be used, particularly given the argument that PCR tests may detect several post-infectious people who have dead virus in their nasal passages but are no longer infectious? How should an organization obtain a CLIA certificate to perform rapid on-site testing, and what are the workflows, logistics, and choice of tests to ensure safe testing and reliable results?
We’ve created a continuously updated peer-reviewed protocol that addresses these issues and other workplace safety questions, providing evidence to specify practical considerations that are not detailed in the CDC or most state guidelines—from the specifics of disinfection to the evidence-base (or lack thereof) for ventilation protection methods. The protocol also details how we established a national testing network to ensure redundant, reliable testing capacity.
While there remains much to be determined about optimal responses to COVID-19, it is clear that the United States’ response to-date has largely been a failure. We can learn from international experiences that rapid, frequent surveillance testing is essential to detecting the approximately 40% of infectious people who have minimal or no symptoms, particularly in high-risk healthcare settings. Implementation of proactive logistics to ensure reliable, frequent testing will be critical to controlling ongoing COVID-19 infections.
Undoubtedly, our hospitals and clinics should have access to systems that can provide optimal testing to their staff and patients; their safety depends on it. Whether hospitals and clinics have the finances to add testing to the costs of PPE is an important consideration, but support from the federal and state governments may be key to implementing this important step in patient and staff safety.
Declaration of interests: Sanjay Basu serves as Vice President of Research & Population Health at Collective Health, which created and maintained the national testing network.
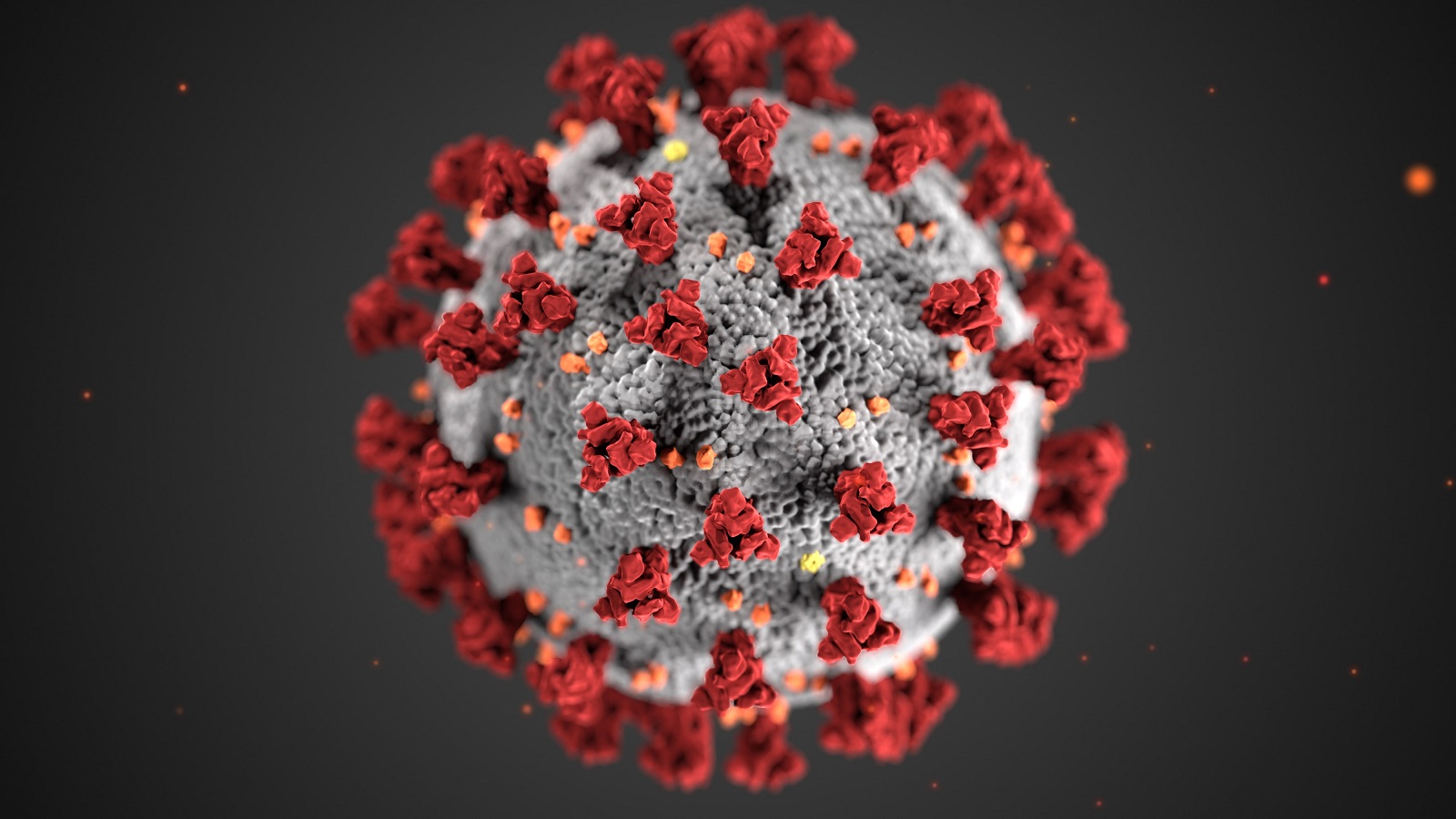
**Feature photo obtained with standard license on Shutterstock.
Interested in other articles like this? Subscribe to our bi-weekly newsletter
Interested in contributing to the Harvard Primary Care Blog? Review our submission guidelines
Sanjay Basu, MD, PhD, is a Primary Care Physician, Epidemiologist, Director of Research at the Harvard Medical School Center for Primary Care, and Vice President of Research & Population Health at Collective Health. His work has focused on preventing and treating chronic diseases, reducing the health effects of financial shocks and other adverse social determinants of health, improving access to essential medicines, and developing primary healthcare infrastructure. He co-founded Possible Health and serves on advisory boards for Columbia University's GRAPH Center, United Nations, World Health Organization, American Heart Association, and Global Burden of Disease Project. Dr. Basu has been named to the "Top 100 Global Thinkers" List by Foreign Policy Magazine and awarded the NIH Director’s New Innovator Award.
- Share
-
Permalink